procedures that have a dramatic impact on a person’s digestive system and health. Dr. Harsh Sheth, a renowned Bariatric Surgeon in Mumbai, specializes in treating conditions that require these types of surgeries. He provides expert guidance and care for patients facing colon and small intestine removal, ensuring they have the best possible outcomes throughout the surgical journey.
Removal of Colon and Small Intestine Symptoms
Removal of the colon or small intestine is usually the last resort when doctors face some medical conditions that negatively affect these organs. The signs accompanying these medical situations differ among patients, but in general, some typical indicators can prompt surgery:
Colon Cancer
Cancer of the colon has the following warning signs:
• Constant and painful sensations in the abdomen
• Altering the pattern of bowel movements, e.g., chronic diarrhea or constipation
• Unaccounted loss of weight
• Blood appearing in the stool
Surgery is frequently the first treatment choice for colon cancer when it is diagnosed at a very early stage. The surgical procedure’s degree will be determined by the tumor’s position and size.
Crohn's Disease
Ulcerative Colitis
Ulcerative colitis, also referred to as another kind of IBD, leads to colon inflammation that lasts for a long time. Among the main symptoms are:
- Diarrhea that is frequent, accompanied by blood
- Extremely painful cramps in the abdomen
- Being very tired
- Getting slimmer
Total colectomy may be necessary when medical treatments do not work or when the risk of colon cancer arises.
Trauma or Injury
Surgical removal of parts of the colon or small intestine may be performed for patients suffering from abdominal injuries resulting from accidents or diseases. Patients generally report the following symptoms:
- Very severe, sudden pain in the abdomen
- Bloating in the abdomen or tenderness
- Blood in the stool
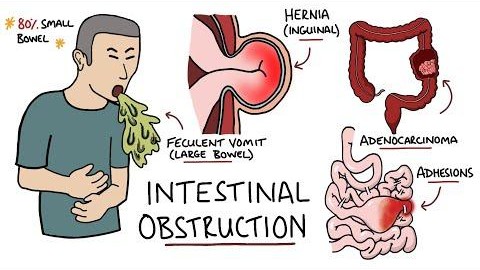
Intestinal Obstruction
When the small intestine is blocked, a person may experience pain, vomiting, and swelling. Sometimes, surgery to remove the part of the intestine that is affected is the solution.
Treatment Options for Colon and Small Intestine Removal

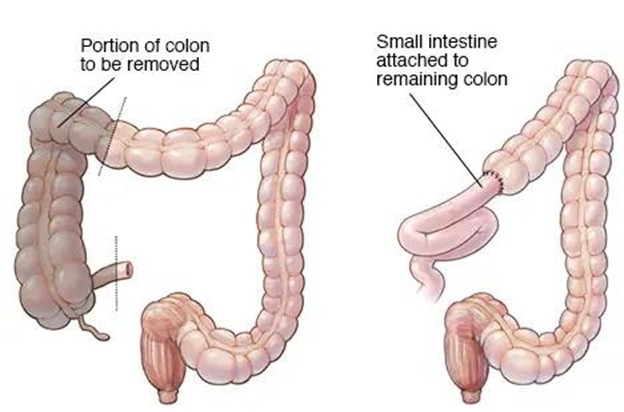
1. Colectomy
Colectomy is the surgery that entails either the complete or the partial resection of the colon.
The various types of colectomies are as follows:
- Partial Colectomy: In this type of surgery, a section of the colon gets removed.
- Total Colectomy: The entire colon is excised. Mostly such kinds of operations are performed when an irrevocable disease, like extensive cancer, or late-stage ulcerative colitis, prevails.
- Subtotal Colectomy: In this operation the rectum and anus are left intact while the rest of the colon is eliminated.
Subsequent to the operation, the patient might be required to undergo an ileostomy or colostomy (which can be either temporary or permanent) to direct the waste away from the body until the healing of the digestive system takes place.
2. Small Bowel Resection
A small bowel resection is a surgical procedure that removes a part of the small intestine that is affected by disease, inflammation, or obstruction. It’s an operation that can bring relief to patients suffering from Crohn’s disease, tumors, or even congenital defects.
- Laparoscopic Surgery: A minimally invasive technique is often preferred for small intestine resections, and this is one such case. The surgical procedure is less traumatic, resulting in a quicker recovery and lighter scars.
- Open Surgery: In special situations, when a large segment of the bowel is affected, traditional open surgery is the only possible option.
3. Ileostomy and Colostomy
A stoma may need to be created on the abdomen to divert feces after a colectomy or small bowel resection; thus, an ileostomy or colostomy may be required. These procedures involve the making of a stoma through which the intestinal waste is divided into a bag located at the abdomen. The ostomy type is determined by the surgery site.
4. Intestinal Transplant
It is not common for intestines to reach the point where they stop performing their functions, and intestinal transplant becomes the only solution; however, such instances do occur. This is one of the most complicated surgery types and is typically done only when the patient has tried all other treatments without success.
Long-Term Outcomes After Colon and Small Intestine Removal

The long-term outcomes after colon and small intestine removal can vary based on the type of surgery, the patient’s overall health, and the condition being treated. Here’s what to expect:
1. Digestive Changes
The most significant impact of these surgeries is on digestion and nutrient absorption. When a large portion of the colon or small intestine is removed, the digestive system may struggle to absorb nutrients effectively. This can lead to:
- Malnutrition: Patients may require nutritional supplements to ensure they’re getting enough vitamins and minerals, especially vitamin B12, iron, calcium, and vitamin D.
- Diarrhea or Constipation: Changes in bowel function are common, especially after a colectomy. Some patients may experience frequent diarrhea, while others may have trouble with constipation.
2. Adjustment Period
It can take time for the digestive system to adapt after surgery. Patients will need to adjust their diet, possibly limiting fiber and introducing small, frequent meals. Probiotics may be recommended to help with gut health.
3. Need for Ongoing Monitoring
Patients who have undergone a colectomy or small bowel resection will need regular follow-up appointments with their healthcare provider to monitor for complications, such as infection, bowel obstruction, or nutritional deficiencies.
4. Potential for Complications
While many patients can live healthy lives after colon or small intestine removal, there are potential long-term complications, including:
- Bowel obstruction
- Chronic diarrhea
- Increased risk of colon cancer (especially after a colectomy for cancer or inflammatory bowel disease)
- Short bowel syndrome (if too much of the small intestine is removed)
Learn more about living with a stoma or managing post-surgery care. Contact Dr. Harsh Sheth for ongoing support and personalized care.
Conclusion
The removal of the colon or small intestine is a significant surgery with both immediate and long-term effects on the digestive system. Whether due to cancer, inflammatory bowel disease, or trauma, understanding the symptoms, treatment options, and possible outcomes of these surgeries can help patients make informed decisions and better prepare for recovery.
If you’re facing the possibility of colon or small intestine removal, Dr. Harsh Sheth, a leading expert in gastrointestinal surgery, can provide comprehensive care and advice tailored to your specific condition.
Ready to learn more about your surgical options? Reach out to Dr. Harsh Sheth today to discuss your personalized treatment plan and recovery strategies.
Frequently Asked Questions
1. Will I need to change my diet after colon or small intestine removal?
Yes, a modified diet will likely be necessary. A nutritionist can guide you on foods that are easier to digest and help manage symptoms like diarrhea or constipation.
2. Can I live without my colon or small intestine?
Yes, many patients lead healthy lives after these surgeries, but they will need to adjust their diet, take supplements, and follow up regularly with their doctor.
3. How soon can I return to normal activities after surgery?
Recovery times vary, but most patients can return to normal activities within 4 to 6 weeks, depending on the extent of the surgery and any complications.
4. What are the risks of colon or small intestine removal surgery?
The risks include infection, bleeding, bowel obstruction, nutritional deficiencies, and complications from anesthesia.
5. Is there any alternative treatment to surgery for conditions requiring colon or small intestine removal?
In some cases, medication, diet, or lifestyle changes can manage the condition, but surgery may still be necessary if other treatments fail.