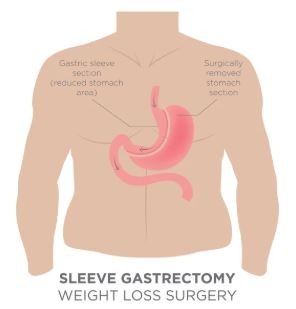
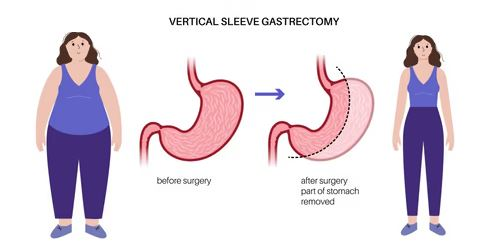
If dealing with overweight is a problem for you and losing weight by conventional methods is impossible, you might turn to surgery as a last resort. Sleeve surgery, more precisely called laparoscopic sleeve gastrectomy, is a minimal invasive procedure in which about 75-80% of the stomach is removed, and a thin “sleeve” is formed which limits the amount of food one can intake drastically.

The modern version of this bariatric operation is laparoscopic surgery, so instead of one large incision, you get several small ones. With the reduction in stomach size, patients not only feel fuller faster but also have their hunger hormones altered, thus, making it easier to keep the weight off permanently—or at least that is the aim.
In the skilled hands of Dr. Harsh Sheth in Mumbai, sleeve surgery can be a real breakthrough in the fight against obesity combined with conditions like diabetes, hypertension, or sleep apnoea. Let’s explore this whole procedure: its mechanism, your expectations, and the actual world of recovery.
Understanding Sleeve Surgery: What It Is and How It Works

Sleeve gastrectomy is where we remove about 80% of your stomach, reshaping it into a slim, banana-like pouch. You end up eating less, and your hunger hormones drop, too. This minimally invasive approach uses a laparoscope, and it’s pretty different from a gastric bypass—which tackles weight loss in another way.
Definition and Overview of Sleeve Gastrectomy
Gastric sleeve surgery is a bariatric operation where we permanently remove a big chunk of your stomach. What’s left is a slim, tube-shaped stomach—think banana-sized, honestly.
“Gastrectomy” just means removing part (or all) of the stomach. In a vertical sleeve gastrectomy, it’s the outer curve that goes, but the pathway for food stays the same as before.
This surgery is irreversible—once that stomach tissue’s gone, it’s gone. The new stomach can only hold about 100-150ml of food, compared to the original 1,500ml (which is a huge difference!).
Some key points
- Permanent reduction of stomach size
- No intestinal rerouting
- Normal digestion is preserved
- Lowered hunger hormones
How Sleeve Surgery Helps with Weight Loss
So, how does this actually help you lose weight? Well, it’s two things: restriction and hormones. With a smaller stomach, you just can’t eat as much at once—simple as that.
Plus, by removing the part of the stomach that makes ghrelin (the “I’m hungry” hormone), your appetite drops. You’re not constantly thinking about your next meal.
The restriction part means you feel full way sooner—sometimes after just 60-80ml of food at first, which is a shock for most people.
Hormonal perks
- Less ghrelin (so, less hunger)
- Better insulin sensitivity
- Improved glucose metabolism
- Boosted satiety hormones
Most folks drop 60-70% of their excess body weight in the first two years. It’s not magic, but it’s pretty dramatic.
Procedure Steps and the Role of the Laparoscope

We do gastric sleeve surgery using laparoscopic techniques. Basically, that means we use a skinny camera and long instruments through tiny incisions instead of opening you up.
Here’s the rough play-by-play:
- Prep – General anaesthesia, patient positioned
- Trocar placement – Five small incisions, each 5-12mm
- Laparoscope in – Camera gives us a clear view inside
- Mobilise stomach – Free up the greater curve
- Stapling – Form the sleeve with surgical staplers
- Tissue out – Remove the extra stomach
- Leak test – Double-check the staple line for leaks
The whole thing usually takes 45-90 minutes. The laparoscope is in play the whole time, helping us be precise and gentle on your tissues.
Recovery’s a lot quicker than traditional open surgery—most people go home within a day or two.
Gastric Sleeve Surgery Versus Other Bariatric Procedures
Gastric sleeve isn’t the only option, but it stands out for being less complex than some alternatives. Unlike gastric bypass, there’s no intestinal rerouting or extra pouch.
Gastric bypass creates a tiny stomach pouch and connects it straight to the small intestine—so you get both restriction and malabsorption.
Biliopancreatic diversion with duodenal switch (bit of a mouthful) is even more involved: it combines a sleeve with a big intestinal reroute. It can lead to the most weight loss, but the risks go up, too.
Procedure | Complexity | Weight Loss | Reversibility |
Gastric sleeve | Moderate | 60-70% | No |
Gastric sleeve | High | 70-80% | Difficult |
Duodenal switch | Very high | 80-90% | No |
Biliopancreatic diversion on its own is rarely done anymore—it just causes too many nutritional headaches. For most people, the gastric sleeve strikes a good balance between real results and manageable risks.
Benefits, Lifestyle Changes, and Aftercare Following Sleeve Surgery
Sleeve gastrectomy can seriously improve obesity-related issues like type 2 diabetes and high blood pressure, but it does mean permanent changes to your eating and supplement habits. If you want lasting results, you’ll need to follow the recommended diet phases and keep up with nutrition checks for life.
Health Conditions Improved by Sleeve Gastrectomy
After sleeve gastrectomy, most people see big improvements in lots of health problems. Type 2 diabetes often comes under control—some folks even go into remission within months.
High blood pressure almost always drops as the weight comes off. Many patients end up lowering or ditching their blood pressure meds (with their doctor’s okay, of course).
Sleep apnoea? That usually gets much better, since less tissue around the neck and throat means fewer airway issues at night.
High cholesterol tends to normalize as people lose weight and eat better, which is a win for your heart.
Joint pain, especially in the knees and hips, often fades as the pressure eases up. You might be surprised how much easier it is to move around without the extra weight.
Acid reflux can improve, though honestly, sometimes it gets worse—so that’s something to keep an eye on with your doctor.
Nutritional Guidelines and Dietary Phases Post-Surgery
Eating after surgery follows a set of phases—each one helps your stomach heal and gets you used to new habits. Usually, you’ll spend 2-4 weeks in each phase, but it really depends on how you’re doing.
Phase 1: Liquid Diet
- Only clear broths and sugar-free drinks
- Helps your stomach heal without stretching
- Staying hydrated is key
Phase 2: Pureed Foods
- Everything needs to be smooth, almost like pudding
- Blended proteins—think cottage cheese or similar
- Skip anything fibrous or with seeds
Phase 3: Soft Foods
- Soft, easy-to-chew foods like soft-boiled eggs
- Tender veggies with no skins
- Start adding more textures, but nothing too toug
Phase 4: Regular Foods
-
- Slowly reintroduce normal textures
- Lean proteinsshould always come first
- Portion control isn’t optional—it’s the new normal
Take your time eating, and chew really well—seriously, it’s more important than you’d think. Chewing well keeps food from getting stuck where your stomach meets your intestine.
Long-Term Lifestyle Changes and Supplement Needs
Life after gastric sleeve surgery is a permanent shift—your eating and lifestyle habits will need to change for good.
Daily Supplements You’ll Need:
- Multivitaminwith iron
- Vitamin B12 (either under the tongue or as an injection)
- Calcium citrate with vitamin D
- Extra iron if your levels are low
These minerals and vitamins help you avoid deficiencies, which can sneak up on you otherwise. Your doctor will want regular bloodwork to keep tabs on everything.
Eating Habits to Adopt:
- Use smaller plates—your portions will be tiny
- Always eat protein first at every meal
- Don’t drink while eating—wait at least 30 minutes before or after
- Aim for 60-100 grams of protein daily
Exercise Guidelines:
- Start with walking or swimming—nothing too intense at first
- Once you’re cleared, add strength training
- Stay active to help prevent weight regain
- Shoot for 150 minutes of moderate activity a week
Expected Outcomes, Limitations, and the Role of Dr. Harsh Sheth
Dr. Harsh Sheth uses minimally invasive techniques for laparoscopic sleeve gastrectomy. With years of bariatric surgery experience, he’s helped many patients dealing with severe obesity find a new path forward.
Typical Weight Loss Results:
- Most folks see 60-70% excess weight losswithin 12-18 months
- The biggest drop usually happens in the first 6 months
- Weight tends to settle and stabilise around 18-24 months after surgery
Potential Limitations
- Weight regaincan happen if lifestyle changes aren’t maintained
- Vitamin deficiencies if you skip supplements
- Some people develop food intolerances
- Surgical risks exist, though they’re quite low with skilled hands
Long-term success really depends on committing to lifestyle changes and having the right support. Dr. Harsh Sheth is there for patients before and after surgery, guiding every step
At the end of the day, the surgery is just a tool. Keeping the weight off is about sticking to nutritional advice and regular follow-ups. We always stress the need for realistic expectations and a lifelong focus on healthy habits.
Conclusion
Sleeve surgery is a proven option for people who’ve struggled with obesity and want significant weight loss. Gastric sleeve patients typically lose 60-70% of their excess weight in that first year to year and a half.
The procedure permanently shrinks the stomach and changes hunger hormones. That’s a big deal, but it only sticks if you’re willing to make real lifestyle changes too.
Key Benefits Include:
- Major weight loss
- Better control over diabetes
- Blood pressure improvements
- Sleep gets better for most people
- More energy and easier movement
We get it—deciding on surgery isn’t easy. Sleeve gastrectomy means a lifelong commitment to new eating habits and regular activity. There’s no shortcut here.
Most folks have fewer complications with this than with other bariatric surgeries. You’re usually back to normal routines in 2-4 weeks, which isn’t too bad.
But honestly, your results hinge on following the post-op game plan. We always suggest working with an experienced nutritionist and maybe a support group or two.
This surgery’s best for those with a BMI over 35 or if you’ve got obesity-related health issues. You’ve got to think it through and be ready for change before jumping in.
Important Considerations:
- The procedure can’t be reversed
- You’ll need to take vitamin supplements
- Regular follow-ups are part of the deal
- There’s always a risk of complications
There’s always the recommendation of having a complete conversation with a skilled bariatric surgeon to determine if sleeve surgery is the perfect option for you and your goals.
Frequently Asked Questions
What is the method for performing a stomach sleeve gastrectomy for obesity treatment?
The surgery of laparoscopic sleeve gastrectomy is done cutting away a large part of the stomach through 4 to 5 small stab wounds made in different places; the remaining part of the stomach then takes the shape of a small tube. The whole process lasts about 1 to 2 hours and it is a permanent fix.
What is the recovery time after the surgery?
Usually, the patient is discharged after 1-2 days, then after a week or two, light work can be done, and full recovery will take 4-6 weeks, during which the patient will gradually progress from liquids to pureed foods and will have to wait for doctor’s higher approval for the consultation.
What are the risks and complications involved in sleeve gastrectomy?
Sleeve gastrectomy does bear some risks such as bleeding, infection, a minuscule chance of the stapled area leaking, thrombosis, reflux, and malnutrition, albeit most of these complications are infrequent with good postoperative care.
Will it be right to say that surgical sleeves are going to be the final solution of obesity problem?
The surgical treatment of obesity by sleeve gastrectomy has a very long-lasting (even for life) effect as it keeps on reducing the appetite hormones and shrinking the stomach so that patients lose 60-70% of their excess weight and the result is no more diabetic—all this maintenance is done through the patients’ lifelong habits.
What criteria must patients meet to be eligible for sleeve gastrectomy?
Candidates usually have a BMI of 35+ (or 30–35 with health problems), are 18–65, have tried other weight-loss options, and are ready for lifelong lifestyle changes, pending a thorough medical assessment.
How does sleeve gastrectomy differ from other forms of bariatric surgery?
Sleeve surgery is simpler than gastric bypass because it doesn’t alter the intestines, offers permanent results compared to balloons, has fewer complications, preserves normal digestion, and usually allows faster recovery.

